Sorry about this morning’s late email, had a bit of technical difficulty. - Noah (NRB)
Noah here. Last December I was visiting my wife’s family for the holidays and I came down with a nasty cold. I had a fever, a bad cough, sore throat, aches, the whole nine yards. After a few days I thought maybe I should stop by an urgent care clinic just to make sure I didn’t have strep throat (with two little kids these things never seem out of the question). I stopped in the day before Christmas and they took a look. The diagnosis was just a bad cold and cough. What I expected to hear next is the regular spiel of drink plenty of fluids and get some rest, but instead they handed me multiple prescriptions. One was a decongestant, which made sense, but the other two were more surprising: a steroid (prednisone) and an antibiotic. The former was to help with nasal passage swelling and the latter was … just in case I didn’t get better? I declined them all, opting to stick with over-the-counters, cough drops, and lots of tea with honey.
Why is this interesting?
I was reminded of the incident after reading yet another piece about drug-resistant bacteria.
Antimicrobial resistance is a major public health threat across the globe, Mkrtchyan notes. Every year, more than 700,000 people die because of it, and the toll is predicted to rise to 10 million by 2050. Resistance means patients will stay sick for longer, which increases the cost of health care, Mkrtchyan says. “Our research highlights that general public areas (part of our everyday life) can be reservoirs for multidrug-resistant bacteria and alerts us that concrete global efforts are required to tackle the problem.”
The over-prescription of antibiotics is a big part of this story and nowhere is this worse, apparently, than urgent care clinics. A 2018 paper that looked at over 150 million doctor’s visits across urgent care, retail clinics (like the ones in pharmacies), emergency departments, and medical offices found that nearly 40% of all urgent care visits ended with prescriptions versus only 7% from a medical office. While clearly some of that difference is attributable to the situation of the visitor, it’s even more exaggerated when the researchers looked at just viral respiratory infections (like the one I had), which they consider “antibiotic-inappropriate.”
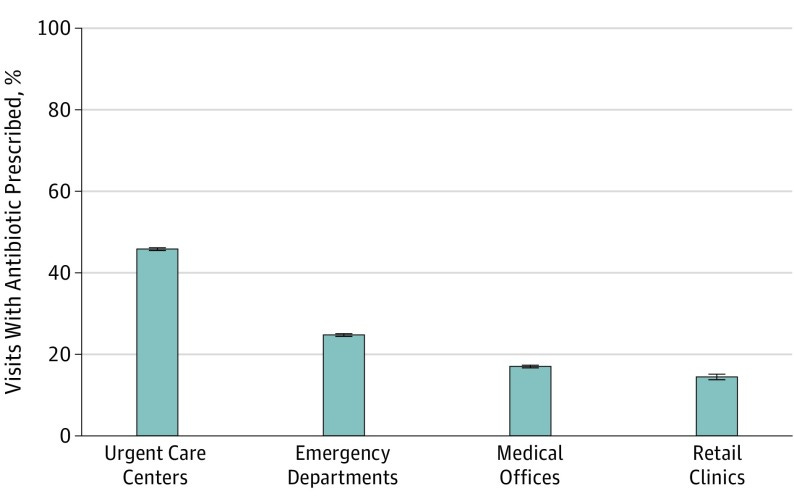
I read into this back in December (I had plenty of time sequestered in bed) and wasn’t particularly surprised. It’s certainly been my experience that nearly every time I step into an urgent care clinic I walk out with a prescription. Part of the reason for that is clearly my own expectation: I’m going because I assume there’s some intervention that can be taken. But, as in the Christmas visit, that’s not always the case. The other side is clearly the role of the clinic itself. It’s a much more transactional relationship than the one you have with your primary care doctor and I assume with that comes some pressure, even if its not explicit, to “deliver value” in the form of drugs. While there’s clearly value to these clinics, particularly as a way to keep folks out of much more expensive emergency rooms, they’re contributing to a very serious public health issue that is only getting worse. (NRB)
Map of the Day:
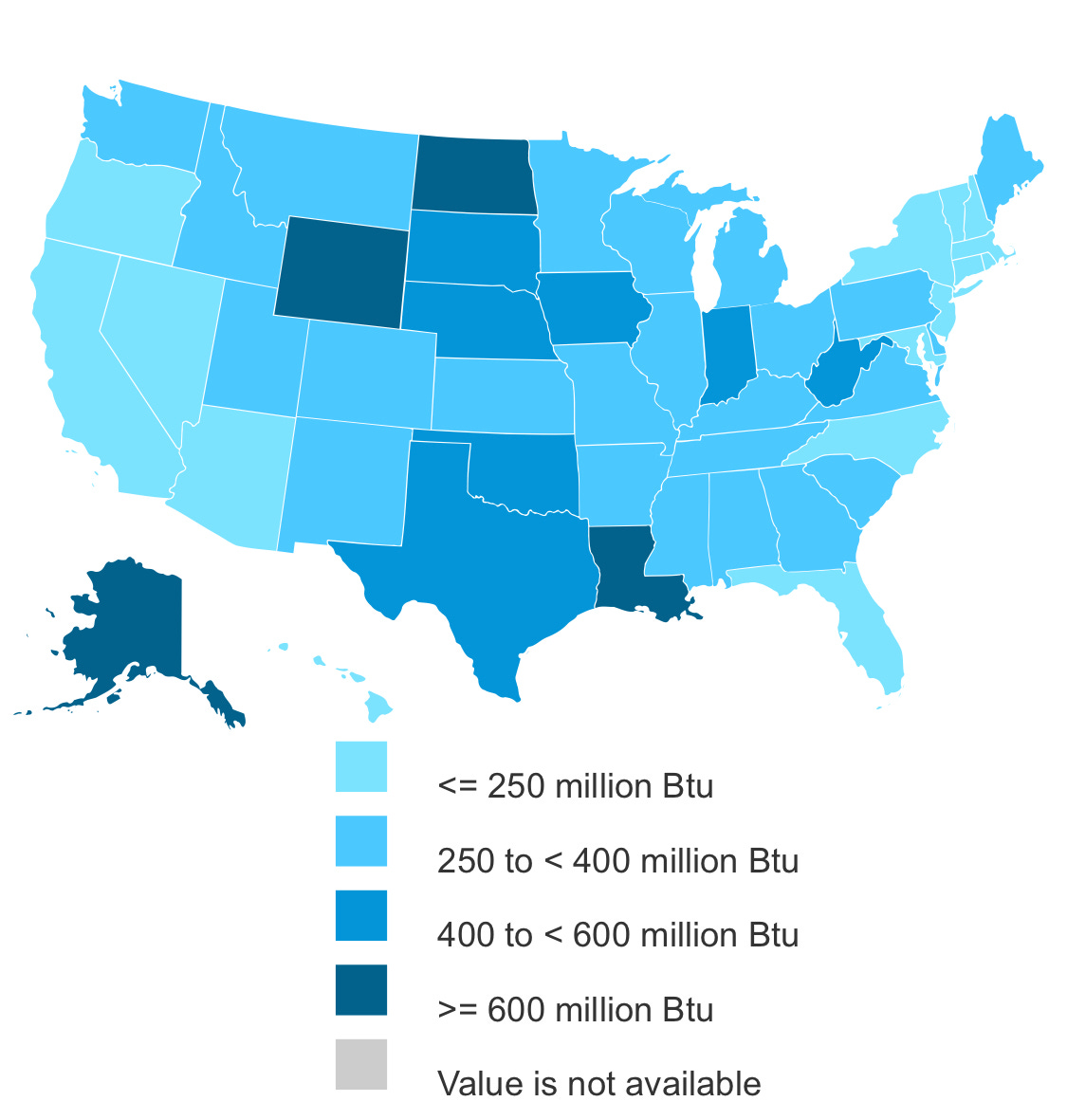
Top energy consuming US states per capita. (NRB)
Quick Links:
New York Times Book Review piece on bibliotherapy, “a term for the psychological benefit patients get from discussing books in a session.” (NRB)
Twitter thread from friend of WITI Abe Burmeister (6/19 - The Extinction Edition) arguing Hudson Yards is a good real estate development. (NRB)
The spycraft revolution. (CJN)
Thanks for reading,
Noah (NRB) & Colin (CJN)


